01 Pages : 1-9
Abstract
Tuberculosis (TB) is a centuries old disease which is quite prevalent throughout the world caused by Mycobacterium tuberculosis. This disease kills more people every year than other infectious diseases despite the existence of an effective treatment. This treatment has been available since 1940, which means its existence spans over more than fifty years now. The development of antimicrobial resistance is one of the challenges facing the struggle to stem the tide of this lethal outbreak. The wider range of this disease is linked to few functional factors which include lack of public awareness, patient monitoring and follow-up. The prevalence of great progress and advancement in medical technology and research calls for greater efforts. This review article considers trends prevailing all around the globe in the ailments from a comprehensive perspective
Key Words:
Mycobacteria Growth Indicator Tube (MGIT960), Drug Susceptibility Testing (DST), Human Immuno Defficiency Virus (HIV), Multidrug-Resistant TB (MDR-TB), Tuberculosis (TB), Extensively Drug-Resistant TB (XDR-TB)
Introduction
TB is known to cause a greater rate of death than HIV and other numerous infections. This whole process starts with the virulence of an extremely contagious and tenacious bacterium. The responsible bacterium is called as Mycobacterium tuberculosis. One major element that contributes is the ability of such microorganisms to create hereditary transformations that bestow protection from various previously powerful antimicrobials. MDRTB and its even more resistant relative, XDR-TB, have gotten to be progressively common since effective anti-microbial medications of TB were discovered. According to some experts, in the next 50 years or so, non-resistant TB will be replaced by MDR-TB as the generally prevailing form of the disease (WHO, 2010)”
However, great success has been achieved in the development of effective techniques and ways for treatment, preventive care, and infection control. Since 1990, the death rate due to TB has decreased around 50% or so and the global health associations are ready to expand this positive effect with same diligence. After a decade of research, it has been stated that “2015 is a watershed moment in the battle against tuberculosis” (World Health Organization (WHO), 2015). The combination of already proven care and administration strategies with new techniques for more efficient recognition as well as treatment of this disease will empower medical care experts to make further progress in winning the battle against this colossal disease. In spite of this achievement, financing for TB control misses the mark concerning that for other irresistible infections. It is unmistakably clear that current financing and loopholes in communication are deteriorating avoidance and control endeavors. But the targeted investments will be fruitful in robust profits in the global campaign to root out the said disease (World Health Organization (WHO), 2015)”
Etiology agent
History of Mycobacterium Tuberculosis Infection
Human beings getting infected by M. tuberculosis has been known all through the history of life. It has emerged from East Africa and transmitted to Europe and Asia as people moved out and it resulted in devastating annihilation for decades all through this world (Frith, 2014). This disease has been termed “phthisis” by the ancient Greeks. Subsequently, the “Great White Plague” of this infection seethed across Europe for over 100 years. Robert Koch had considered this malady incurable and lethal round the clock during all that time. The etiology of tuberculosis was also explained by him to the Berlin physiological society and afterwards, he was awarded Nobel Prize in 1905 on presenting his discoveries. This led to the dawn of an era of exceptional advances in the remedy and nullification of this lethal infectious ailment. (Daniel, 2006).
Pathogenesis
M. tuberculosis is an airborne pathogenic microbe. The alveolar macrophages quickly swallow the M. tuberculosis once they enter the alveoli via airborne droplets carrying the pathogen. The complement system (C3 protein) plays an essential role in the engulfment of microbe (Van Crevel, Ottenhoff and Van Der Meer, 2002). The phagocytosis results in a chain of events that lead to either likely control of the disease (latent tuberculosis) or may progress to dynamic illness, called primary progressive tuberculosis.
After being phagocytosed, the bacteria multiply in number gradually, with cell division cycle happening every 25 to 32 hours. At first, there is generation of proteolytic enzymes and cytokines by the macrophages to debase microscopic organisms. T lymphocytes are drawn to this site by the cytokines; leading to the cell-mediated immunity. T cells get themselves attached to the bacterial antigens presented on the surface of the macrophages. This process of immune system proceeds for 2 to 12 weeks; the mycobacteria keep multiplying to fully whip up the cell-mediated response (Dheda et al., 2005). The people with intact cell-mediated immunity develop granulomas around the mycobacteria in their defense. Ghon complexes (nodular sort lesions) are composed of aggregates of T lymphocytes and macrophages and they limit replication and the spread of the microbes. The destruction of macrophages causes necrosis at the lesion site, but the microbes still manage to sustain themselves since they can change their phenotypes to improve endurance. The necrotic environment starts resembling caseous necrosis in 2 to 3 weeks, having soft cheese like appearance whose conditions include restricted supplements and low pH making the lesions go through calcification and fibrosis letting the microbes enter a dormant form (du Toit, Pillay and Danckwerts, 2006).
Culture and Sensitivity
The bacterium is able to withstand traditional gram staining, so normally an alternative stain (Ziehl-Neelsen) is used instead. It is an acid-fast stain whics shows the potential of M. tuberculosis to retain carbolfuchsin stain by culturing them on Lowenstein-Jensen media for 8 weeks (Brennan and Nikaido, 1995)
“It can also be diagnosed by symptoms, chest radiography and findings from the tuberculin (Mantoux) skin test (Prevention, 2013) (Goering et al., 2019). Signs and symptoms of TB include cough lasting longer than normal, coughing up sputum, pain in chest, weight loss, chills, pyrexia, fatigue, and night sweats (CDC, 2018). TB can also be revealed by any parenchymal, nodal or pleural abnormality on chest radiograph (Leung, 1999). These test findings can be further confirmed through microscopic findings of acid fast bacteria.”
“Another way to detect TB is known as the interferon-gamma release test (IGRA) which measures the body's immune response to mycobacterium by blood tests (Prevention, 2013). Particularly, it measures interferon-gamma levels when blood cells interact with an antigen from bacterium. Subsequently, it requires further testing to determine the type of TB disease.”
“The presence of drug resistance during treatment also needs to be determined. Resistance to INH (Isoniazid) and Rifampin is confirmed by the detection of mutation in the catalase gene and the RNA polymerase gene respectively. The luciferase test can detect significantly drug-resistant strains (Levinson, 2014).”
Treatment and Prognosis
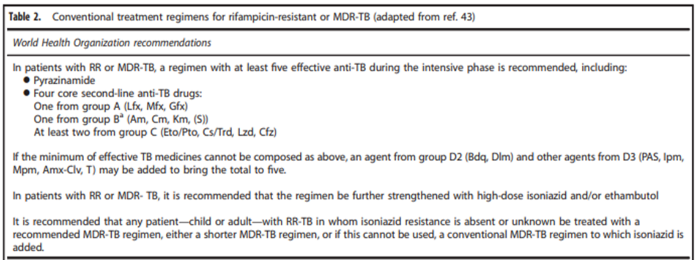
The treatment of inactive tuberculosis (CDC, 2012) includes Isoniazid, rifapentine and rifampin currently. For now, 10 FDA approved drugs for the treatment of active TB. Ethambutol, and pyrazinamide forms the core treatment regimen for TB (CDC, 2012). The 6-month regimen consists of isoniazid, rifampin, and pyrazinamide given for 2 months followed by isoniazid and rifampin for 4 months. The success rate with the 6-month regimen in sputum transformation is beyond 90% inside the primary two months of treatment. It is important to complete the drug treatment because if the treatment is stopped prematurely, the bacteria will remain active and become non-resistant to the first-line drugs to overcome this situation, supervision of the physician and patient follow-up become necessary (Brode et al., 2015).”
Epidemiology
Vulnerable Populations
People are at risk of contracting TB and these people have HIV-positive and various psychiatric patients 2QAZ. People living in poverty and with a higher incidence of the disease are at greater risk. Weak people are at a lower social and economic levelSome of the factors contributing to this risk include delayed and inaccurate diagnosis, unavailability of treatment, and ignorance or denial of symptom significance (Kawatsu and Uchimura, 2016). Globally, strategies such as targeted public awareness campaigns, access to accurate diagnostic, and therapeutic skills are being used to increase the effectiveness of TB control units.”
Antibiotic Resistance
One of the major hurdles in the fight against tuberculosis is the development of resistance against the drug that is used to treat it (Sanyaolu, 2019).
Multiple-Drug Resistant Strain
Multiple-drug resistant strains of tuberculosis are resistant to isoniazid and rifampin which are both first line drugs. The catalase-peroxidase enzyme, which is inscribed by the kat G gene of M. tuberculosis, is involved in triggering the Isoniazid pro-drug. This activation of isoniazid will form an acyl radicle of isonicotinoyl interacting with NADH or NAD to form adduct of isoniazid-NADH. This adduct of isoniazid-NADH is a strong blocker of inh-A which is a gene that will form an enoyl acyl-carrier protein reductase that will further produce mycolic acids. Genetic mutations in kat G can lead to resistance of isoniazid as they are unable to activate the isoniazid prodrug, blocking their effect (Sanyaolu, 2019).
Rifampin inhibits RNA-synthesis which is DNA-based. It inhibits bacterial RNA polymerase which is DNA based. The drug Rifampin will bind to RNA polymerase at the adjacent side of active center of RNA polymerase which will block the phosphodiester bond formation by blocking RNA-synthesis in RNA backbone [52, 53]. Rifampin resistance forms from the mutation which will alter the small fragments of the binding sites of rifampin on the RNA polymerase causing a reduced affinity of rifampin and will minimize its effects (Sanyaolu, 2019).
Extensive-Drug Resistant Strain
XDR strains are resistant to fluoroquinolones (for example “ofloxacin and moxifloxacin”) and to one of the three second-line drugs (which are injectables including amikacin, capreomycin or kanamycin). All XDR mechanisms are not described. Fluoroquinolones are derived from nalidixic acid. The acid derivatives will then inhibit a topoisomerase protein which is involved in the super-coiling of DNA by interfering with bacterial DNA replication. Fluoroquinolones Resistance forms when there is a development of mutations in the genes of bacteria called gyr A and gyr B, Resistance to other second-line TB drugs includes ethionamide, macrolide (clarithromycin) (Sanyaolu, 2019)
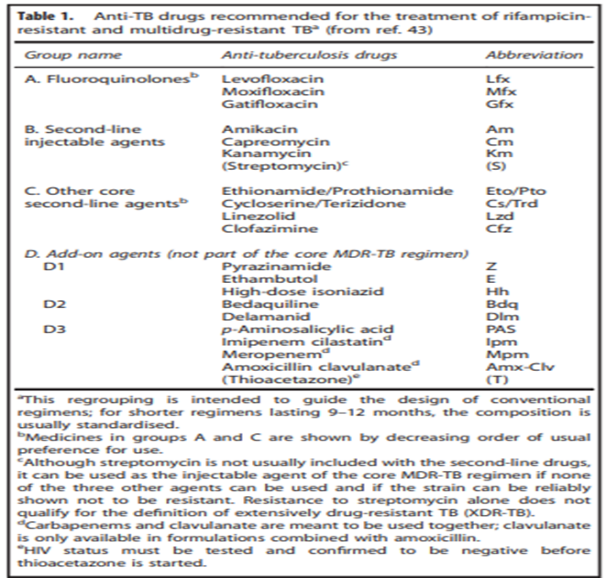
A preview of the last classifications of the anti-tb drugs in which 5 groups are present where 1st group contains first line drugs and group 2 have 2nd line drugs.
Prevention and Control
Treatment for the latent TB infection has been divided into 2 different important group by WHO i.e. individuals infected with HIV, and children under the age of 5 years who can be in contact at home with someone with certified TB (Sanyaolu, 2019).
Development of the different tools to give rapid and efficient screening of the drug-resistant strain of bacteria is one of the most important strategy to control the disease. Other very important factor is the communication between health care givers. Modern and upgraded hospitals and clinics, and public education will help control the disease (Sanyaolu, 2019) .
A serious problem in today’s TB is the slow detection of bacterial strains which are drug resistant. The areas where MDR-TB and XDR-TB is found are the most under-developed areas and they have no access to modern TB diagnostic tools and health care facilities.Patient gets inappropriate treatment in such cases where susceptibility of bacteria is not known This will maximize the chances of death of the patient from TB and cause resistance to many other broad spectrum antibiotics (Sanyaolu, 2019).
Currently, the most used test these days is drug susceptibility testing (DST) of TB which is works through the automatic system called as the BACTEC MGIT960 which cultures and identifies the mycobacterial strain by doing the analysis of DNA. Different test kits are being used which detect resistance of the strain and identifies the bacterial strain which are drug resistant in almost every patient (Sanyaolu, 2019).
Other plan to control the infection of TB is to improve construction of healthcare centers in areas where TB outburst is more. In many underdeveloped areas, hospitals are overcrowded, and structure of building is such that it is difficult to quarantine the TB-infected patients. This is especially important in places where there is more HIV patient as they are at high risk to TB infection. To control the disease Public and patient awareness of TB is very important. For these policies to be affective, funds and investments are needed for human resources, personnel, community outreach programs, transportation and equipment delivery (Sanyaolu, 2019).
New Advances in the Treatment of TB
Novel Derivatives
Novel Fluoroquinolones
Gatifloxacin and Moxifloxacin are of vital importance for the treatment of TB as they have higher activity than ofloxacin, sparfloxacin, Ciprofloxacin, and levofloxacin
Ciprofloxacin has been reported to have the least bactericidal activity. levofloxacin and ofloxacin had greater activities whereas gatifloxacin and moxifloxacin were reported to have the greatest activities (Hu, Coates and Mitchison, 2003).
Moxifloxacin
It interferes with the protein synthesis to slowly metabolize the bacteria by a mechanism that is different from other drugs like rifampin. Improved activity is obtained by inhibition of effluxes leading to a build-up of higher concentrations (Pestova et al., 2000)(Coyle, Kaatz and Ryba, 2001)(Daporta et al., 2004)
Gatifloxacin
Gatifloxacin is known to have greater activity in preclinical studies and is more likely to be cross-resistant to moxifloxacin. With identical activity to moxifloxacin, therapeutic indications early of gatifloxacin’s anti-TB activity are promising. Although, in pregnant woman and in children the drug has not been detected.
Gemifloxacin
It is a quinolone that has shown great results in many phase 3 trials. With the oral bioavailability of 70%, it is well-tolerated and has 7.4 hrs of elimination half-life. It is suitable for a once-daily dosing regimen(Allen et al., 2001). Studies show that even at the highest lethal dose, it would not be effective for the treatment of TB(Ruiz-Serrano et al., 2000).
Sitafloxacin
Sitafloxacin has outstanding activity against a broad spectrum of bacteria. It is able to suppress DNA gyrase and topoisomerase IV equally (Tomioka et al., 1999)
Newer Rifamycin Derivatives
Rifabutin and Rifapentin
According to the MIC, rifabutin (RBT) is effective than rifampin for MTB for almost four to eight times for example tissue penetration and long shelf life. Centers for Disease Control (CDC)recommended use of rifapentine instead of rifabutin to treat active TB in HIV patients. RPT is two to four times more effective than RIF compared to MTB and also has a better pharmacokinetic profile than RIF(Bemer-Melchior, Bryskier and Drugeon, 2000)(Mor et al., 1995). Due to the high serum level and partial elimination, RPT has a much longer time to act than other rifamycin derivatives (Keung et al., 1999).
Rifalazil
It is a new semi-synthetic rifamycin, has a longer elimination half-life and is much more effective against M. tuberculosis (Shoen, DeStefano and Cynamon, 2000). Be that as it may, viruses that are resistant to high levels of rifampicin - show resistance to all rifamycins (Moghazeh et al., 1996). In any case, because of the severe side effects in Phase II trial, the improvement of rifalazil has been discontinued.
Macrolides
Clarithromycin (CAM) works compared to MTB only in very strong in-vitro environments, much larger than its Cmax levels in lungs tissues and serum in humans and therefore cannot be clinically achieved (Truffot-Pernot et al., 1995). CAM can therefore be given simultaneously to improve effectiveness of these drugs in the treatment of MDR-TB with first anti-TB drugs.
Clofazimine
Clofazimine (CFZ), a riminophenazine antimycobacterial agent, is used widely in the leprosy’s treatment. CFZ shows significant anti-MTB activity in both in vivo and in vitro in preoperative studies. Due to its excellent anti-MTB activity, it is often incorporated into MDR-MTB treatment regimens. However, oral CFZ was found to be less effective compared to intracellular MTB when used alone or administered in combination with the drugs like EMB & PZA in the MDR-TB treatment.
Mikasome
Amikacin belongs to aminoglycoside used as anti-TB drug (second-line agent)(Allen et al., 1983). The anti-mycobacterial activity of an embedded liposome drug is effective in combating Mycobacterium infections in vitro and animal models. Mikasome has been shown to resolve M infections in Pilot Phase II studies. (Davis et al., 2007)
5-Nitroimidazole
The dormant form of mycobacterium is resistant to common anti-mycobacterial agents such as isoniazid & rifampicin (Dick, 2001). Metronidazole is the first drug that has been shown to work against an inactive tubercle acting as a prodrug as it is low in redox energy to a small body that is at risk of forming a central nitro group that damages DNA and causes subsequent cell death(Murugasu-Oei and Dick, 2000). patients receiving metronidazole have shown clinical improvement based on improved doses that reduce the amount of sputum and significant radiographic improvement (Desai et al., 1989)
Nitroimidazopyran PA-824
PA-824, a leading compound belongs to nitroimidazopyrans (“made on the basis of 5-nitroimidazole CGI 17341”) is extremely effective for treatment of MDR-MTB and shows bactericidal action against MTB(dormant) (Stover et al., 2000). It shows strong bactericidal activity against MTB mostly due to its suppressive action on lipid and proteins synthesis by MTB organisms after it activates with the cofactor-dependent MTB F-420 (Barry, Boshoff and Dowd, 2005). It is not cross-resistant to some of the first drugs to fight TB.
Linezolid
Linezolid is oxazolidinone that works by inhibiting protein synthesis and is active against drug-resistant strains of M. tuberculosis. (1) linezolid by interfering with complex formation inhibits ribosomal protein synthesis and leading to premature inhibition of protein synthesis and resistance to antimicrobial agents, (2) a wide range of substances including a significant number of bacterial species, (3) a low level of the emergence of non-resistant mutations, and (4) a completely self-contained element, and there is no natural storage resistance (5) superior oral and parentral bioavailibility (B. and P.C., 2004). Linezolid is not resistant to other antimicrobial agents.
Pleuromutilins
Pleuromutilins works by inhibiting the growth of M-tuberculosis and has been shown to interfere with the protein mycobacterial synthesis (by binding 23S r RNA) , in this way it prevents the synthesis of peptide bond (Schlünzen et al., 2004). The GSK-TB Alliance is currently operating on Pleuromutilins based on pleuromutilins that work against MDR-TB and are effective enough to reduce the length of existing TB treatment.
Progress in Research and Development
For the annual reduction in global incidence of TB, the advancement in technology is needed and those areas which needs to be focused is: vaccines that cause reduction of infection, vaccines/drugs that reduce the chance of infection in newly infected people, rapid diagnostic method that is used in care and other short and simple treatment options. Though we need development in research, but the progress of development is very slow especially in diagnostic technology that emerged in 2017 despite current increase in TB research and development funding. According to (WHO, 2018) there are 20 drugs, 12 vaccines and several treatment methods which are under clinical trial.
Conclusion
Although there are advancements in research and technology and as well as development in many antiretroviral drugs, but M. Tuberculosis infection is still the world’s largest infectious disease. There are funding’s for research and development, but the funding’s are for other diseases. The strategies which have proven to control the disease is advancement in diagnostic tool, patient’s management in effective way, identification and managing the germs which are drug resistant. The international committee has made a strong commitment to encompass these clinical strategies and remove this deadly disease
References
- Allen, A. et al. (2001). ‘Multiple-dose pharmacokinetics and tolerability of gemifloxacin administered orally to healthy volunteers', Antimicrobial Agents and Chemotherapy. doi: 10.1128/AAC.45.2.540- 545.2001.
- Allen, B. W. et al. (1983). 'Amikacin in the treatment of pulmonary tuberculosis', Tubercle. doi: 10.1016/0041-3879(83)90035-1.
- B., B. & P.C., A. (2004). 'Oxazolidinones: Activity, mode of action, and mechanism of resistance', International Journal of Antimicrobial Agents.
- Barry, C., Boshoff, H. & Dowd, C. (2005). 'Prospects for Clinical Introduction of Nitroimidazole Antibiotics for the Treatment of Tuberculosis', Current Pharmaceutical Design. doi: 10.2174/1381612043383214.
- Bemer-Melchior, P., Bryskier, A. & Drugeon, H. B. (2000). ‘Comparison of the in vitro activities of rifapentine and rifampicin against Mycobacterium tuberculosis complex', Journal of Antimicrobial Chemotherapy. doi: 10.1093/jac/46.4.571.
- Brennan, P. J. & Nikaido, H. (1995). 'The envelope of mycobacteria', Annual Review of Biochemistry. doi: 10.1146/annurev.bi.64.070195.000333.
- Brode, S. K. et al. (2015). ‘Multidrug-resistant tuberculosis: Treatment and outcomes of 93 patients', Canadian Respiratory Journal. doi: 10.1155/2015/359301
- Brogden, R. N. & Fitton, A. (1994). ‘Rifabutin: A Review of its Antimicrobial Activity, Pharmacokinetic Properties and Therapeutic Efficacy' Drugs. doi: 10.2165/00003495- 199447060-00008.
- Cambau, E. & Drancourt, M. (2014). ‘Steps towards the discovery of Mycobacterium tuberculosis by Robert Koch, 1882', Clinical Microbiology and Infection. doi: 10.1111/1469-0691.12555.
- Campbell, E. A. et al. (2001).'Structural mechanism for rifampicin inhibition of bacterial RNA polymerase', Cell. doi: 10.1016/S0092- 8674(01)00286-0.
- Catanzaro, A. et al. (2015). 'Performance comparison of three rapid tests for the diagnosis of drug- resistant tuberculosis', PLoS ONE. doi: 10.1371/journal.pone.0136861.
- CDC. (2018) Tuberculosis (TB) Disease: Symptoms and Risk Factors, Centers for Disease Control and Prevention. CDC, C. for disease control and prevention (2012). 'TB Elimination (Multidrug- Resistant Tuberculosis (MDR TB))', Cdc.
- Coyle, E. A., Kaatz, G. W. & Ryba, M. J. (2001). 'Activities of newer fluoroquinolones against ciprofloxacin-resistant Streptococcus pneumoniae', Antimicrobial Agents and Chemotherapy. doi: 10.1128/AAC.45.6.1654- 1659.2001.
- Van Crevel, R., Ottenhoff, T. H. M., & Van Der Meer, J. W. M. (2002). 'Innate immunity to tuberculosis', Clinical Microbiology Reviews.
- Daniel, T. M. (2006) 'The history of tuberculosis', Respiratory Medicine. doi: 10.1016/j.rmed.2006.08.006.
- Daporta, M. T. et al. (2004). 'In vitro activity of older and newer fluoroquinolones against efflux- mediated high-level ciprofloxacin-resistant Streptococcus pneumoniae', International Journal of Antimicrobial Agents. doi: 10.1016/j.ijantimicag.2004.01.012.
- Davis, K. K. et al. (2007). 'Aerosolized amikacin for treatment of pulmonary Mycobacterium avium infections: An observational case series', BMC Pulmonary Medicine. doi: 10.1186/1471-2466- 7-2.
- Desai, C. R. et al. (1989). 'Role of metronidazole in improving response and specific drug sensitivity in advanced pulmonary tuberculosis.', The Journal of the Association of Physicians of India.
- Dheda, K. et al. (2005). 'Lung remodeling in pulmonary tuberculosis', Journal of Infectious Diseases. doi: 10.1086/444545.
- Dick, T. (2001). 'Dormant tubercle bacilli: The key to more effective TB chemotherapy [3]', Journal of Antimicrobial Chemotherapy. doi: 10.1093/jac/47.1.117.
- Ducasse-Cabanot, S. et al. (2004). 'In Vitro Inhibition of the Mycobacterium tuberculosis β-Ketoacyl- Acyl Carrier Protein Reductase MabA by Isoniazid', Antimicrobial Agents and Chemotherapy. doi: 10.1128/AAC.48.1.242- 249.2004.
- Feklistov, A. et al. (2008). ‘Rifamycins do not function by allosteric modulation of binding of Mg 2 to the RNA polymerase active center', Proceedings of the National Academy of Sciences of the United States of America. doi: 10.1073/pnas.0802822105.
- Fischer, B., & Ferlinz, R. (1995). 'Therapy and prognosis of tuberculosis', Versicherungsmedizin / herausgegeben von Verband der Lebensversicherungs- Unternehmen e.V. und Verband der Privaten Krankenversicherung e.V.
- Frith, J. (2014). 'History of tuberculosis. Part 1 - Phthisis, consumption and the white plague', Journal of Military and Veterans' Health.
- Goering, R. V. et al. (2019). MIMS Medical Microbiology and Immunology, Journal of Visual Languages & Computing.
- Hu, Y., Coates, A. R. M., & Mitchison, D. A. (2003). 'Sterilizing activities of fluoroquinolones against rifampin-tolerant populations of Mycobacterium tuberculosis', Antimicrobial Agents and Chemotherapy. doi: 10.1128/AAC.47.2.653-657.2003.
- Kawatsu, L., & Uchimura, K. (2016). 'Tuberculosis annual report 2014 -(1) Summary of statistics on tuberculosis notification and foreign-born tuberculosis patients', Kekkaku.
- Keung, A. et al. (1999) ‘Single and multiple dose pharmacokinetics of rifapentine in man: Part II', International Journal of Tuberculosis and Lung Disease.
- Leung, A. N. (1999). 'Pulmonary tuberculosis: The essentials', Radiology. doi: 10.1148/radiology.210.2.r99ja34307.
- Levinson, W. (2014). Review of Medical Microbiology and Immunology, The effects of brief mindfulness intervention on acute pain experience: An examination of individual difference.
- Merle, C. S. et al. (2014) ‘A Four-Month Gatifloxacin- Containing Regimen for Treating Tuberculosis', New England Journal of Medicine. doi: 10.1056/nejmoa1315817.
- Milatovic, D. et al. (2000). 'In vitro activities of sitafloxacin (DU-6859a) and six other fluoroquinolones against 8,796 clinical bacterial isolates', Antimicrobial Agents and Chemotherapy. doi: 10.1128/AAC.44.4.1102- 1107.2000.
- Moghazeh, S. L. et al. (1996). ‘Comparative antimycobacterial activities of rifampin, rifapentine, and KRM-1648 against a collection of rifampin-resistant Mycobacterium tuberculosis isolates with known rpoB mutations', Antimicrobial Agents and Chemotherapy. doi: 10.1128/aac.40.11.2655.
- Mor, N. et al. (1995). 'Comparison of activities of rifapentine and rifampin against Mycobacterium tuberculosis residing in human macrophages', Antimicrobial Agents and Chemotherapy. doi: 10.1128/AAC.39.9.2073.
- Murugasu-Oei, B. and Dick, T. (2000). ‘Bactericidal activity of nitrofurans against growing and dormant Mycobacterium bovis BCG', Journal of Antimicrobial Chemotherapy. doi: 10.1093/jac/46.6.917.
- Pestova, E. et al. (2000) ‘Intracellular targets of moxifloxacin: A comparison with other fluoroquinolones', Journal of Antimicrobial Chemotherapy. doi: 10.1093/jac/45.5.583.
- Prevention, C., & for, D. C., (2013). 'Core Curriculum on Tuberculosis : What the Clinician Should Know', Centers for Disease Control and Prevention National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention Division of Tuberculosis Elimination.
- Quemard, A., Lacave, C., & Laneelle, G. (1991). ‘Isoniazid inhibition of mycolic acid synthesis by cell extracts of sensitive and resistant strains of Mycobacterium aurum', Antimicrobial Agents and Chemotherapy. doi: 10.1128/AAC.35.6.1035.
- Ramaswamy, S., & Musser, J. M. (1998). ‘Molecular genetic basis of antimicrobial agent resistance in Mycobacterium tuberculosis: 1998 update', Tubercle and Lung Disease. doi: 10.1054/tuld.1998.0002.
- Rouse, D. A. et al. (1995). 'Characterization of the katG and inhA genes of isoniazid-resistant clinical isolates of Mycobacterium tuberculosis', Antimicrobial Agents and Chemotherapy. doi: 10.1128/AAC.39.11.2472.
- Rozwarski, D. A. et al. (1998). 'Modification of the NADH of the isoniazid target (InhA) from Mycobacterium tuberculosis', Science. doi: 10.1126/science.279.5347.98.
- Ruiz-Serrano, M. J. et al. (2000). 'In vitro activities of six fluoroquinolones against 250 clinical isolates of Mycobacterium tuberculosis susceptible or resistant to first-line antituberculosis drugs', Antimicrobial Agents and Chemotherapy. doi: 10.1128/AAC.44.9.2567-2568.2000.
- Schlünzen, F. et al. (2004). 'Inhibition of peptide bond formation by pleuromutilins: The structure of the 50S ribosomal subunit from Deinococcus radiodurans in complex with tiamulin', Molecular Microbiology. doi: 10.1111/j.1365-2958.2004.04346.x.
- Scior, T. et al. (2002). 'Antitubercular isoniazid and drug resistance of Mycobacterium tuberculosis - A review', Archiv der Pharmazie. doi: 10.1002/ardp.200290005.
- Shoen, C. M., DeStefano, M. S., & Cynamon, M. H. (2000). ‘Durable cure for tuberculosis: Rifalazil in combination with isoniazid in a murine model of Mycobacterium tuberculosis infection', Clinical Infectious Diseases. doi: 10.1086/313876.
- Slayden, R. A., & Barry, C. E. (2000). ‘The genetics and biochemistry of isoniazid resistance in Mycobacterium tuberculosis', Microbes and Infection. doi: 10.1016/S1286- 4579(00)00359-2.
- Stover, C. K. et al. (2000). 'A small-molecule nitroimidazopyran drug candidate for the treatment of tuberculosis', Nature. doi: 10.1038/35016103.
- du Toit, L. C., Pillay, V., & Danckwerts, M. P. (2006). 'Tuberculosis chemotherapy: Current drug delivery approaches', Respiratory Research. doi: 10.1186/1465-9921-7-118.
Cite this article
-
APA : Faiz, R., Chaudary, K., & Saeed, R. (2019). Recent Advances in the Treatment of Tuberculosis Infection. Global Immunological & Infectious Diseases Review, IV(I), 1-9. https://doi.org/10.31703/giidr.2019(IV-I).01
-
CHICAGO : Faiz, Ravish, Khansha Chaudary, and Rabia Saeed. 2019. "Recent Advances in the Treatment of Tuberculosis Infection." Global Immunological & Infectious Diseases Review, IV (I): 1-9 doi: 10.31703/giidr.2019(IV-I).01
-
HARVARD : FAIZ, R., CHAUDARY, K. & SAEED, R. 2019. Recent Advances in the Treatment of Tuberculosis Infection. Global Immunological & Infectious Diseases Review, IV, 1-9.
-
MHRA : Faiz, Ravish, Khansha Chaudary, and Rabia Saeed. 2019. "Recent Advances in the Treatment of Tuberculosis Infection." Global Immunological & Infectious Diseases Review, IV: 1-9
-
MLA : Faiz, Ravish, Khansha Chaudary, and Rabia Saeed. "Recent Advances in the Treatment of Tuberculosis Infection." Global Immunological & Infectious Diseases Review, IV.I (2019): 1-9 Print.
-
OXFORD : Faiz, Ravish, Chaudary, Khansha, and Saeed, Rabia (2019), "Recent Advances in the Treatment of Tuberculosis Infection", Global Immunological & Infectious Diseases Review, IV (I), 1-9
-
TURABIAN : Faiz, Ravish, Khansha Chaudary, and Rabia Saeed. "Recent Advances in the Treatment of Tuberculosis Infection." Global Immunological & Infectious Diseases Review IV, no. I (2019): 1-9. https://doi.org/10.31703/giidr.2019(IV-I).01
